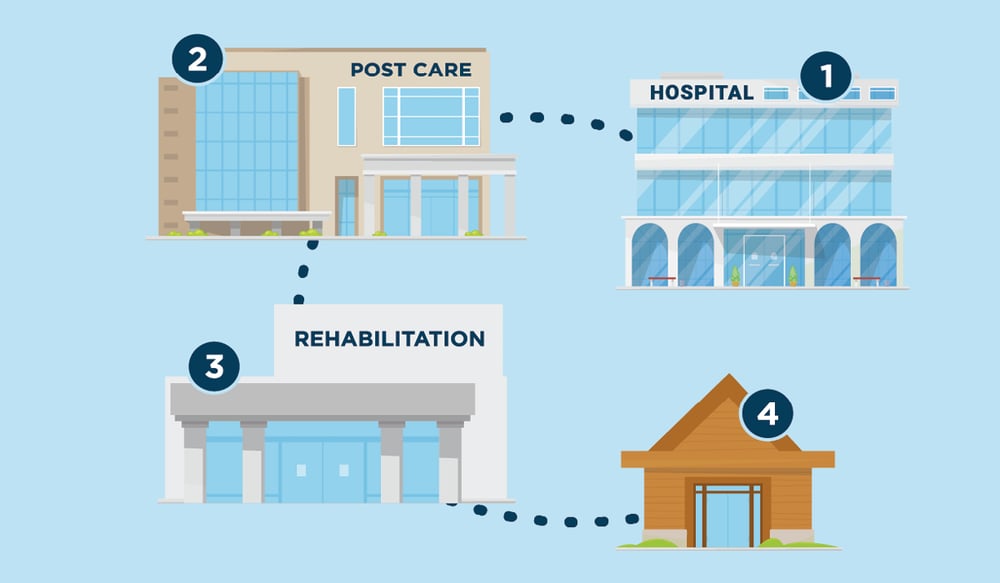
In a continuum of care, the concept of an integrated care system, there are many risks for patient safety. Let’s explain that with an example:
The patient who needs surgery to have her left hip replaced is a 72-year-old woman with moderate Alzheimer’s disease and Type 2 diabetes. To her family and friends, she’s the source of hugs, home-cooked meals, and timeless advice.
A breakdown in communication between her pre-operative nurse and the surgical team about urinary tract infections, for example, could result in an incident or poor surgical outcome. Similarly, lack of understanding about in-home fall risks could trigger an adverse event—and that could require an additional inpatient stay, a delayed recovery, and higher healthcare costs.
Clear lines of communication between the surgery team and the patient’s primary care provider and their family member can help avoid adverse events. All of this information must be documented in the electronic health record (EHR) and shared electronically with the patient’s entire care team. The goal of this holistic planning? This patient’s hip surgery is not just a standalone procedure. It’s part of a continuum of care—or a comprehensive care plan—that adjusts to the needs of this patient over time. It addresses various aspects and levels of care and includes, but isn’t limited to, her medical needs. It is a practical roadmap to ensure patient safety.
>> Learn more about the importance of communication in our blog "The essence of communication in patient safety".
What is meant by the continuum of care?
In healthcare, the continuum of care is the concept of an integrated care system, in which the patient is central and is guided through every subsequent step. Over time, the patient goes through various parts of the system, depending on the phase of the treatment or the need for care. For example, the term is used to describe how healthcare providers follow a patient from preventive care, through medical incidents, rehabilitation, and maintenance.
Its importance lies in its ability to enable healthcare organizations and providers to evolve care with the patient over time, to ensure quality, and to fill any care gaps. It recognizes that a patient's health may be vulnerable or negatively impacted during gaps in care and during transitions (e.g., to a home or post-acute facility).
Often, seven basic categories are cited within the continuum of care, including extended care, acute hospital care, ambulatory care, home care, outreach, wellness, and housing.
Coordination across the continuum of care
Regardless of the post-operative plan, it’s important to ensure that everyone on the patient’s care team is informed appropriately, and that handoffs occur to avoid any potential risks.
The discharge process is a key part of the continuum of care—and a vital opportunity for patient education. For example, common discharge instructions provided to patients might include the following:
- Home care, such as taking pain medications as prescribed, refraining from driving, and making an appointment to have staples removed within two weeks
- Incision care, such as observing the wound for any changes, preventing infection through hand-washing, and refraining from showering for five to seven days
- Sitting and sleeping, which includes using chairs with arms and not sitting for more than 30 to 45 minutes at a time
- Moving safely, which can include using a cane, crutches, or a walker and doing prescribed exercises
- Follow-up, such as making an appointment as advised by a healthcare provider
Key throughout the continuum of care—in physical therapy, pain management, and discharge to the home or a rehabilitation facility—is making sure that everyone has access to the appropriate information about the patient. This reduces the likelihood of adverse events that can result in untreated pain or, for example, a fall at home because of ill-positioned electrical cords.
The teach-back technique
Healthcare teams must invest time to ensure the patient understands her surgical plan and if she’ll be sent home or to a rehabilitation facility for recovery, and when that will occur. Awareness of cultural and language barriers, in addition to any cognitive challenges, is also an important part of the care continuum.
The use of the teach-back technique helps to ensure patients and their family members understand the surgical procedure and the recovery process, in addition to mobility and pain management. This technique helps translate medical terminology, regardless of the patient’s education level.
The teach-back Quick Guide, developed by the U.S. Agency for Healthcare Research and Quality, advises the following:
- Use the teach-back method with all patients.
- Start with the most important message the patient needs to hear.
- Limit the communication to two to four main points.
- Rephrase the message until the patient demonstrates that they understand it.
Examples of phrases a clinician can use to ensure the patient understands include: “Just to be safe, I want to make sure we are on the same page. Can you tell me…?” or “Can you show me how you would use your inhaler at home?”
Patients with dementia or Alzheimer’s present unique challenges. But a background paper published by the U.S. Department of Health and Human Services in 2017 concluded that care coordination can help older adults with chronic conditions, including those with dementia. According to the paper, it’s important to address sources of fragmentation and inefficiencies in care delivery, which then improves the quality of care and health outcomes for patients and their caregivers.
Clinicians should coordinate with a surrogate when a patient with dementia can’t make decisions on their own, in particular with medical procedures such as surgery, according to the Alzheimer’s Association. Failure to incorporate these principles could result in a lack of understanding about the patient’s care plan, mobility, or pain management, which could delay their recovery. Clear and documented communication across clinicians and family members or friends across the continuum of care can help ensure fewer adverse events.
Technology and continuum of care
Throughout the continuum of care, healthcare organizations are presented the opportunity to focus on person-centered care: Patients and their families have a unique perspective, and their direct feedback should always be taken seriously. The fast and accurate follow-up to complaints, for example, can turn a negative experience into a positive one for the patient, and aid the healthcare organization in fostering a good reputation and avoiding the high costs of possible claims.
Today’s technology allows feedback to be easily collected through an online form or file. The progress of each case is monitored throughout the continuum of care and, where appropriate, brought to the attention of management through notifications and reports.
Across the continuum of care, unfortunately, there will always be risks, big and small. Help foster quality and risk management at your organization to control these risks and eliminate them as much as possible.
More information about patient safety in an integrated care chain?
- Our eBook about safety culture in healthcare tells you more about how improving the culture will help increase patient safety.
- Check our blog "Make healthcare safer with system-wide incident reporting".
- Learn more about our software solutions for the reporting of incidents and complaints.

%20(3)%20(1).jpg)


